Physical Therapy for Runners
in Arlington, VA
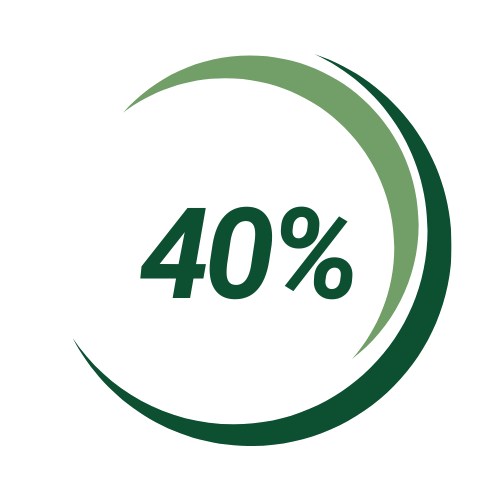
Number of runners injured in a given year
Number of injured runners who give up running
Too Many Injured Runners?
Every year, 8-32% of runners will give up running due to an injury. Runners deserve better from the healthcare system. Too often, runners are told to simply “stop running” instead of being offered a realistic, proactive plan to recover and return - it’s no surprise that many runners avoid seeking care altogether.
At Persist Physical Therapy, I understand what running means—physically, mentally, and emotionally—and I’m here to guide you back with clarity, confidence, and a plan built around your goals. My mission is not to sideline people, but to keep you running— even as we work to build you up stronger than before.
With so many injuries - why even run?
Running isn’t just exercise. It’s a stress reliever, a social outlet, and for many of us, an identity. As both a physical therapist and a runner, I get what it feels like to be sidelined, and I know how powerful it is to feel strong and confident in your stride again.
Running also comes with huge physical and mental benefits:
Despite the myth, recreational running actually protects your joints, with studies showing lower rates of hip and knee osteoarthritis in recreational runners compared to sedentary individuals (Alentorn-Geli et al., 2017)
Lower risk of cardiovascular death and all-cause mortality (Pedisic et al., 2020)
Improved mood, cognitive function, and sleep (Schuch et al., 2016)
In other words, running is good for you—and I’m here to help you keep it that way.
My Approach
I don’t do cookie-cutter care, and I don’t rush you through a crowded clinic. At Persist, you’ll work one-on-one with a licensed physical therapist who’s also a runner—someone who understands both the science and the mindset behind endurance sport.
Here’s how I’ll help you get back on track:
Strength Training
Research shows that strength training can reduce injury risk by up to 85% in runners (Desai et al., 2023). We focus on evidence-based loading strategies that support tissue capacity, improve force absorption, and build long-term durability.
Gait Retraining
Small changes in cadence, trunk lean, or footstrike can dramatically reduce load on injured structures. We use video gait analysis and guided cueing to help you run more efficiently and with less pain (Chan et al., 2018).
Load Management & Coaching
Training errors are one of the biggest causes of injury. I use a collaborative approach to help you fine-tune your mileage, intensity, and rest to prevent overload while keeping you progressing toward your goals.
Modalities to Support Progress
Sometimes pain needs to be calmed before progress can be made. We use dry needling, cupping, and taping techniques strategically—not as a crutch, but as a bridge to active rehab when symptoms limit movement.
The “Big Six” Running Injuries
Most running injuries aren’t sudden—they’re the result of overload, when the stress placed on your tissues exceeds your body’s ability to adapt. This mismatch can come from:
- Sudden increases in mileage or intensity
- Poor sleep, nutrition, or recovery
- Weakness, fatigue, or past injuries
Gait inefficiencies
Training surface or footwear issues
Understanding and addressing both the cause and the contributing factors is the key to meaningful recovery—and that’s exactly what we do at Persist PT.
Click Below to find out more
-
Runner’s knee is one of the most common injuries I see in both new and experienced runners. It often presents as pain around or behind the kneecap, especially with stairs or squatting. At Persist PT, I assess the root cause—often involving quad strength, gait mechanics, and training volume—and build a personalized plan that includes strength progression, taping if needed, and smart return-to-run guidance.
-
If you’re dealing with sharp, lateral (outside) knee pain—especially when running downhill—you might be facing IT band syndrome. This condition is closely tied to hip strength and running mechanics. I use lateral hip strengthening, gait retraining, and soft tissue techniques (like dry needling and foam rolling) to reduce irritation and improve movement patterns so you can return to running pain-free.
-
Shin splints often show up when runners increase mileage too quickly or return from time off. I help runners identify contributing factors like cadence, foot mechanics, and gait. Treatment includes load management, strength work for the lower leg and hips, and running form tweaks that reduce stress on the shins and prevent progression to stress fractures.
-
Bone stress injuries require a strategic rehab plan—rushing back too soon increases the chance of progression to a stress fracture. I help runners safely rebuild load tolerance with gradual progressions, strength training, cross-training support, and education on energy availability and recovery. When needed, I coordinate with referring physicians for imaging and clearance before return-to-run.
-
Achilles pain is common in runners, particularly those doing hill work and speed sessions or when transitioning to a forefoot strike pattern. At Persist PT, I focus on progressive tendon loading, calf strength, and gait retraining (like adjusting foot strike or vertical oscillation). I also use dry needling and manual therapy when appropriate to support tissue recovery and get you back to running strong.
-
That first-step-in-the-morning pain is often a hallmark of plantar heel pain (plantar fasciitis). Whether you're a high-mileage runner or coming back from time off, I work with you to reduce symptoms through mobility, foot and calf strengthening, gait adjustments, and footwear guidance. I also use taping and soft tissue techniques to offload the area so you can stay active during rehab.

Book a Free 15-Minute Discovery Call
Schedule a 15-minute call with a Doctor of Physical Therapy.